A method for 3D bioprinting eye tissues utilising patient stem cells has been developed by researchers at the National Eye Institute (NEI) in the United States. The researchers claim that by using their method, which involves printing three different kinds of immature choroidal cells onto a biodegradable scaffold, it would be possible to produce an endless supply of tissues taken from patients. These, in turn, may enable medical professionals to comprehend the underlying mechanisms of prevalent degenerative retinal illnesses like age-related macular degeneration (AMD).
“Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases,” said Marc Ferrer, Ph.D., Director of the 3D Tissue Bioprinting Laboratory at NIH’s National Center for Advancing Translational Sciences. “Such tissue models have many potential uses in translational applications, including therapeutics development.”
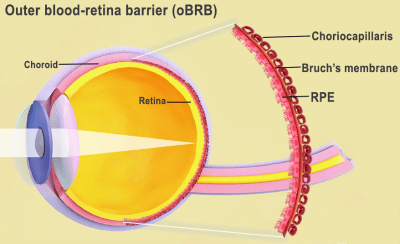
AMD, which essentially causes patients’ central vision to become blurry, is brought on by a number of things, including ageing, heredity, high blood pressure, and nutritional problems. The extracellular matrix (ECM), or Bruch’s membrane, which is situated between the retina and the choroidal capillaries of the eye, is thought to be the origin of these triggers for the formation of lipoprotein deposits known as drusen.
The retinal pigment epithelium (RPE) in the outer blood-retina barrier eventually breaks down as a result of this condition, which also hinders the membrane from controlling nutrients and waste around the eye and causes vision loss. The causes of AMD are well established, but how it progresses is still rather mysterious.
“We know that AMD starts in the outer blood-retina barrier,” explained Kapil Bharti, Ph.D., who heads the NEI Section on Ocular and Stem Cell Translational Research. “However, mechanisms of AMD initiation and progression to advanced dry and wet stages remain poorly understood due to the lack of physiologically relevant human models.”
Bharti and his colleagues have developed a method for 3D bioprinting tissues from patient stem cells in an effort to advance studies on AMD progression.
In this method, fibroblasts, which provide tissues structure, are joined with pericytes and endothelial cells, essential capillary components, to create a new hydrogel.
Then, a scaffold capable of sustaining cell development is printed using this gel.
“By printing cells, we’re facilitating the exchange of cellular cues that are necessary for normal outer blood-retina barrier anatomy,” added Bharti. “For example, the presence of RPE cells induces gene expression changes in fibroblasts that contribute to the formation of Bruch’s membrane – something that was suggested many years ago but wasn’t proven until our model.”
The manufacturing of several other optical medical procedures has used conventional 3D printing, whereas the 3D bioprinting of eye tissues is yet in the experimental stage.
Using 3D printing and augmented reality (AR) glasses, physicians at the Israeli Galilee Medical Center (GMC) created a method of treating eye socket fractures in 2021.
3D APAC Pty Ltd Copyright © 2023. All rights reserved